Seafood allergies are a serious and potentially life-threatening condition affecting millions worldwide. Whether you’re allergic to fish, shellfish, or both, understanding the causes, symptoms, and prevention strategies is crucial for managing your allergy safely. This comprehensive guide will cover everything you need to know about seafood allergies, including diagnosis, myths, and emergency preparedness.
What Causes Seafood Allergies?
Seafood allergies occur when the immune system mistakenly identifies certain proteins in fish or shellfish as harmful, triggering an allergic reaction. The primary allergens are:
- Tropomyosin – Found in shellfish like shrimp, crab, lobster, and mollusks (oysters, clams, and squid).
- Parvalbumin – The main allergenic protein in fish, commonly found in species like salmon, tuna, and cod.
Fish vs. Shellfish Allergies: What’s the Difference?
- Shellfish Allergy: Primarily caused by tropomyosin, common in shrimp, crab, lobster, and mollusks.
- Fish Allergy: Triggered by parvalbumin in bony fish like cod, salmon, and tuna.
- Cross-Reactivity: People allergic to one type of seafood may not necessarily be allergic to the other since their allergens differ. For instance, those allergic to shrimp may still tolerate fish, as shellfish allergens (tropomyosin) are distinct from fish allergens (parvalbumin).
Symptoms of Seafood Allergies
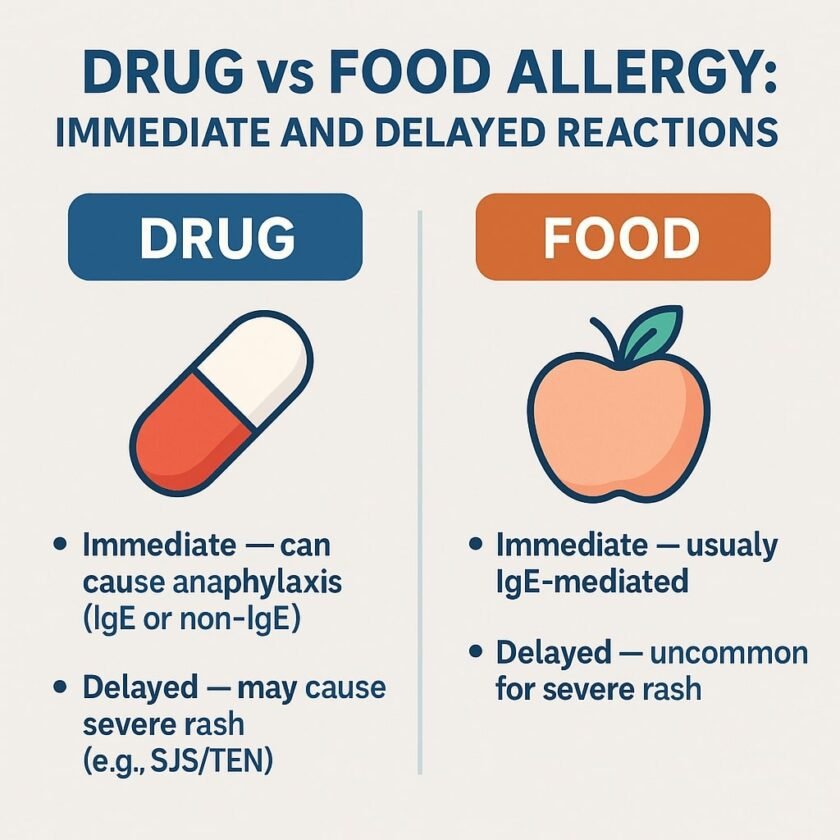
Allergic reactions can occur within minutes to a few hours after consuming seafood. Symptoms range from mild to severe and may include:
Mild Symptoms:
- Itchy skin or hives
- Swelling of lips, face, or tongue
- Stomach pain, nausea, or vomiting
Severe Symptoms (Anaphylaxis):
- Difficulty breathing or wheezing
- Throat swelling or tightness
- Dizziness, rapid heartbeat, or low blood pressure
- Anaphylactic shock, requiring immediate treatment with an epinephrine auto-injector (EpiPen) and emergency medical attention
Can Seafood Allergies Develop Later in Life?
Yes! Some people eat seafood for years without issues and suddenly develop an allergy. Known as adult-onset food allergy, this phenomenon is believed to result from changes in the immune system over time. Seafood allergies are typically lifelong and require a proper diagnosis for confirmation.

Diagnosing Seafood Allergies
If you suspect a seafood allergy, consult an allergist for testing. Common diagnostic methods include:
- Skin Prick Test: Detects immediate allergic reactions to seafood proteins.
- Blood Test (Specific IgE): Measures immune response to seafood proteins.
- Oral Food Challenge (Under Medical Supervision): Involves consuming small amounts of seafood to assess reactions.
- Component-Resolved Diagnostics (CRD): Identifies specific proteins causing reactions to help predict severity and cross-reactivity.
Note: At-home allergy tests are unreliable. Always seek professional medical advice.
Managing and Preventing Seafood Allergies
While there’s no cure for seafood allergies, proper management can help you avoid reactions. Here’s how:
1. Avoiding Hidden Seafood Allergens
Seafood proteins can be found in unexpected places, such as:
- Asian sauces (oyster sauce, fish sauce). Patients with seafood allergies may be safer using alternatives such as soy sauce, but it’s essential to check the ingredient label, as some brands may add seafood-derived ingredients.
- Processed foods (soups, seasonings, pizza toppings)
- Supplements & Medications: Glucosamine, which is commonly derived from shellfish shells, is generally safe for individuals with shellfish allergies since it does not contain allergenic proteins. However, those with severe allergies should consult their healthcare provider before use. Plant-based or synthetic glucosamine alternatives are also available.
2. Cross-Contamination Prevention
- Use separate utensils and cookware for seafood-free meals.
- Inform restaurant staff about your allergy when dining out.
- Avoid shared cooking surfaces and fryers.
3. Emergency Preparedness
- Always carry an EpiPen if you have a history of severe reactions.
- Wear a medical alert bracelet indicating your allergy.
- Educate family and friends on how to respond in an emergency.
4. Traveling with a Seafood Allergy
- Carry a doctor’s note and allergy translation cards when traveling.
- Research local emergency services and hospitals.
- Avoid high-risk cuisines that commonly use seafood ingredients.
Common Myths About Seafood Allergies
Myth #1: Iodine Causes Seafood Allergies
Fact: Seafood allergies are caused by proteins, not iodine. People with seafood allergies can safely undergo iodine-based medical procedures.
Myth #2: Cooking Destroys Seafood Allergens
Fact: Heat does not break down the proteins responsible for seafood allergies. Even fully cooked seafood can trigger reactions.
Myth #3: Fish Oil Supplements Trigger Fish Allergies
Fact: Most fish oil supplements are purified and do not contain allergenic proteins. However, individuals with severe allergies should consult an allergist before use.
Myth #4: Imitation Crab is Safe for Shellfish Allergies
Fact: Imitation crab often contains real shellfish extract, making it unsafe for those with shellfish allergies.
Scombroid Poisoning vs. Seafood Allergy
Not all reactions to seafood are due to allergies. Scombroid poisoning occurs when fish (e.g., tuna, mackerel, mahi-mahi) is improperly stored, leading to bacterial production of histamine.
Symptoms of Scombroid Poisoning:
- Skin flushing
- Headache
- Nausea and vomiting
- Heart palpitations
- In severe cases, difficulty breathing and low blood pressure
Unlike true seafood allergies, mild to moderate scombroid poisoning is treated with antihistamines. However, in severe cases, epinephrine may be necessary, and emergency medical attention should be sought immediately.
Final Thoughts
Seafood allergies can be severe and require careful management. By understanding the differences between fish and shellfish allergies, recognizing symptoms, and taking proactive steps to avoid exposure, individuals can reduce their risk of allergic reactions.
Key Takeaways:
✔ Know the symptoms and seek immediate help for severe reactions. ✔ Get tested by an allergist for accurate diagnosis. ✔ Always carry an EpiPen and inform others about your allergy. ✔ Take precautions when dining out or traveling. ✔ Don’t believe common myths—stay informed with evidence-based information.